When should I get a Total Hip Replacement?
Our hip joints can deteriorate or become damaged through a multitude of reasons, including repetitive stress, auto-immune disorders, and traumatic injuries.
A damaged hip joint can manifest in people in numerous ways, including pain, weakness, and decreased range of motion.
Every patients’ tolerance to their deficits and the impacts of those deficits on their life are different. If you feel like your hip pain is becoming unbearable and you’re finding yourself unable to do the things you need or love, then you should reach out to a hip specialist to discuss your options.
A hip specialist will typically gather your medical history and perform a physical examination to determine the next step. Often, the next step is to try a course of physical therapy, even before ordering additional diagnostic imaging like X-rays, MRIs, or CT scans.
This is because even with severe joint deterioration, physical therapy can help improve pain, strength, and mobility, which can delay or potentially avoid the need for surgery all together. At the very least, even if surgery becomes necessary, physical therapy will have helped improve post-surgical outcomes through its pre-surgical intervention.
If a patient isn’t progressing as expected with physical therapy, then the hip specialist may consider trying other conservative treatments such as pain-relieving injections (PRP, Cortisone) or medications.
However, based on the patients’ own preferences and results with other interventions, the hip specialist may then suggest getting a total hip replacement.

What are the different types of hip replacement surgeries?
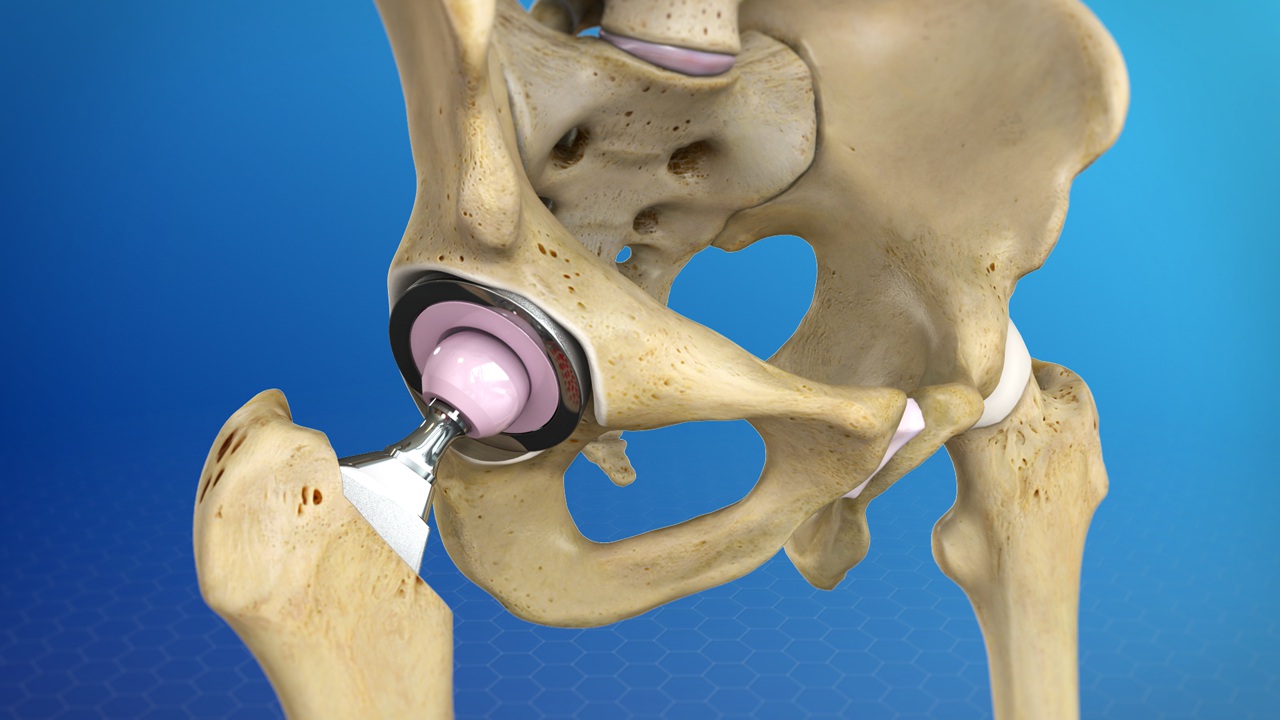
The types of hip replacement surgeries are mainly differentiated by the direction the surgeon is approaching the hip joint from. The 4 most common hip replacement approaches are posterior, direct lateral, anterior-lateral, and anterior. The direction of approach primarily affects the size of the incision and the muscles/tendons that will need to be maneuvered around to perform the replacement, all of which affects recovery time and outcomes.
Historically the posterior approach was the most common type of total hip replacement, because it allowed for the largest view and workspace for the surgeon to perform the procedure. However, as techniques and technology have become more sophisticated and precise, the anterior approach has become more popular since it allows for a smaller incision and less disruption of the surrounding anatomy.
This results in the patient experiencing less pain, more mobility with lower risk of dislocation, faster recovery times, and allows for the procedure to be done in an outpatient environment rather than inside a hospital.

How long is the recovery after a hip replacement?
With a posterior hip approach, the recovery time before full weight bearing and return to normal ambulation is typically around 6-8 weeks.
The anterior hip approach has greatly reduced this recovery time, down to 3-4 weeks.
Most anterior hip replacement patients can be weight bearing without pain within the first 1-3 weeks. However, because the hardware is not secured with cement within the bone in this procedure, surgeons typically recommend using an assistive device, such as a walker or a cane during the first 3-week period to give time for the new bone formation to integrate with the hardware.

Will I be able to fully return to all my activities after my hip replacement?
One of the best predictors of how well your functional outcomes will be after a total hip replacement is how functional you are going into your surgery. Which is why physical therapy is important to do even before you go into the operating room.
Full return to high-level activities, including running and jumping, after a total hip replacement has certainly been achieved by several patients. However, these aggressive impact activities can shorten the lifespan of the hardware, which may then require another surgical procedure to replace. The replacement procedure for a total hip replacement is called a “revision”. Revisions typically have significantly lower functional outcomes compared to the initial total hip replacement, which is why many surgeons recommend avoiding these high-impact activities.
Nevertheless, weighing out the risks of a revision and the value of these high-level activities in the end is a decision that the patient needs to make.
Our team of physical therapists value educating our patients on the different considerations that need to made with their decision, and then guiding them on what would be the best approach to achieve whichever goals they want to move forward with.
Michael Domingo, DPT, OCS

This post was written by Dr. Michael Domingo in March of 2022.
Learn more about Mike on our about page: https://gopt.co/people/michael-domingo/
Special thanks to Dr. Laura Matson Ko for contributing to this article. Dr. Laura Matsen Ko is a Seattle based Board Certified Orthopedic Surgeon, specializing in Hip & Knee Joint Reconstruction. You can learn more about Dr. Laura Matsen Ko on her website at https://www.lauramatsenkomd.com/